Canine–mediated human rabies has the highest case fatality rate of any known infectious disease and kills approximately 59,000 people annually, mostly children, with millions more saved only by costly post–exposure prophylaxis (PEP). The vast majority of human rabies fatalities occur in Africa and Asia, where access to PEP is limited.
To draw attention to this neglected disease, the Washington State University Paul G. Allen School for Global Animal Health (Allen School) has joined the commitment made by the World Health Organization (WHO), the Food & Agricultural Organization (FAO) and the World Organization for Animal Health (OIE) to eliminate this disease by 2030 (‘Zero by 30’).
While human rabies can be effectively prevented with PEP, the intervention is expensive, and for poor people living in remote communities, access to healthcare is often constrained by social, geographical and economic factors. Consequently, in countries with endemic rabies, the burden associated with the disease is considerable.
Mass dog vaccination (MDV) is an efficient approach to eliminating human rabies by inoculating the reservoir host responsible for more than 99% of human infections. As seen in the United States where wildlife reservoirs still exist, domestic dog vaccinations have all but eliminated human rabies. However, implementing MDV across the rural landscapes where rabies remains endemic is logistically challenging and expensive. As a result many countries spend substantial resources providing PEP with limited investment in MDV, and human deaths continue to occur at an unacceptably high rate.
Despite the dearth of MDV projects, rabies has several epidemiological features that make elimination through MDV possible:
- Domestic dogs, not wildlife, are responsible for more than 99% of human rabies cases.
- The basic reproductive ratio (R0 —the number of secondary infections produced from a primary case) of canine rabies is low (~1.2).
- The low R0 means that vaccination coverage only needs to be maintained above 20 – 45% to control rabies and eliminate ongoing transmission, including to all other secondary hosts such as wildlife, livestock and humans.
- Despite the appearance of being stray, the vast majority of domestic dogs in sub–Saharan Africa have some form of ownership and are accessible to parenteral vaccination.
Because of these aforementioned features, MDV provides a feasible means to eliminate human rabies. To this end, the Allen School has been collaborating with organizations in Tanzania, Kenya and the UK to devise novel cost-effective MDV delivery strategies that can be delivered at scale to enable regional, national and, eventually, continental elimination of rabies.

To eliminate rabies on a regional scale, these once–per–year campaigns must vaccinate at least 70% of each community’s dog population to maintain the minimum coverage above 20 – 45% throughout the year.
Because dogs in these areas are rarely vaccinated privately, the proportion of immunized dogs begins to fall as soon as each campaign ends. The result of the birth of unvaccinated puppies and previously immunized dogs dying typically leads to fluctuating coverage.
Decentralized, community–led delivery strategies are a promising way of improving access to health interventions and have been used in Africa for the control of neglected tropical diseases such as onchocerciasis. In the case of rabies, it has been hypothesized that a community–led model will improve coverage consistency and reduce delivery costs. Despite these potential benefits, community–led approaches have not been evaluated for the control of rabies.
The barrier to implementing and testing community–led interventions has been the inability to store rabies vaccines under cold–chain conditions in rural communities. The availability of a thermo-tolerant rabies vaccine that can be stored without loss of potency for extended periods at temperatures exceeding cold–chain conditions would allow the investigation of community–led delivery options.
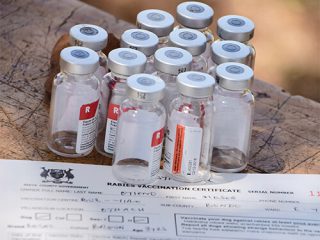
In 2016, WSU carried out the first field based trial to investigate whether a commonly used rabies vaccine (Nobivac® Rabies) would remain potent following extended storage at temperatures outside of cold-chain conditions. The results of this trial (doi.org/10.1016/j.vaccine.2016.10.015) indicated that the vaccine remained potent following storage for six months at 25°C and for three months at 30°C. These exciting results, indicating that the rabies vaccine can be stored outside of refrigeration units for extended periods without the loss of potency, will likely catalyse the development of novel delivery strategies.
For example, WSU’s follow–on study in northern Tanzania is investigating whether recruiting and training village–based Rabies Coordinators, responsible for storing vaccines within their communities and implementing MDV campaigns year round, will be a more cost–effective approach for achieving the consistent levels of coverage required for regional elimination.


